Video Library
Filter
Keyword Search
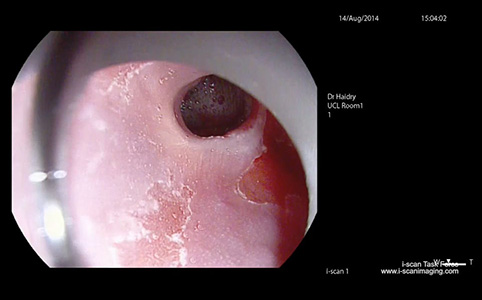
Intramucosal cancer in Barrett`s Oesophagus (Zoom IMC)
This short video shows the exciting new magniview gastroscope in use. This is a patient with a previous Barrett’s Cancer that was resected. At first inspection there appears to be residual flat Barrett’s oeosphagus. However a combination of i-scan and acetic acid shows an area at the right wall with featureless mucosa and abnormal irregular micro-vasculature with zoom endoscopy. One can appreciate the normal adjacent villous mucosa next to the featureless area of intramucosal cancer that was resected by EMR.
Courtesy of Dr. Rehan Haidry, UCLH, UK

Colonoscopy with one detected polyp in the transverse colon
The video shows 49 year old male with suspected food allergy. During colonoscopy, one polyp in the transverse colon was detected. The histology showed a lymphoid follicle and tubular adenoma with LGIEN.
Two aspects in the lesion, the central pit pattern is almost invisible under white light endoscopy and comes out much clearer under i-scan 1 (surface enhancement for detection) and i-scan 2 (tone enhancement for characterization).
Courtesy of Prof. Timo Rath from Erlangen University Hospital, Germany

Colonoscopy with two detected polyps
The video shows a colonoscopy of a 31 year old male with suspected food allergy. During the colonoscopy two polyps were found:
- one tubular adenoma with LGIEN in the descending colon
- one tubular adenoma with LGIEN in the sigmoid colon
The lesion can be easily missed with white light endoscopy (WLE), also in the setting of a very young patient.
By using i-scan 1, a better demarcation is possible. The vascular pattern are almost invisible unless i-scan OE is used.
Courtesy of Prof. Timo Rath from Erlangen University Hospital, Germany

Colonoscopy with detected Tubular Adenoma with LGIEN and SSA polyps
The video shows a screening colonoscopy of a 71 year old female. Two polyps were found during the screening:
- one tubular adenoma in the cecum
- one sessile serrated Adenoma (SSA) in the ascending colon. The pit pattern of polyp number two is almost not visible under white light endoscopy but comes out with i-scan (Type II open). Since SSA show accelerated progression towards CRC, i-scan really helps to differentiate them from hyperplastic lesions.
Courtesy of Prof. Timo Rath from Erlangen University Hospital, Germany

Advanced endoscopy imaging and therapy in the colon – the dawn of an exciting era
Barcelona, Spain 2017
Courtesy of Prof. M Iaccucci, Birmingham, UK

Image guided endoluminal therapy in Barrett’s esophagus: advanced imaging for detection and decision making
Barcelona, Spain 2017
Courtesy of Prof. R. Bisschops, Leuven, Belgium

Testimonial 1 - Dr. Erik van der Heijden
Courtesy of Dr. Erik van der Heijden, Radboud University Mediacl Centre Nijmegen, The Netherlands

Benefits of i-scan in Pulmonology
Experiences on i-scan
Courtesy of Dr Erik van der Heijden, Radbound University Medical Centre Nijmegen, The Netherlands

Mucosal inflammation, healing and dysplasia in IBD: “A new era of enhanced endoscopic imaging”
Lisbon, May 10th 2016
Courtesy of Prof. Marietta Laccuci, University of Calgary, Canada

Optical Imaging (i-scan OE), the newest imaging technology for driving endoscopic therapy in the lower GI tract
Lisbon, May 10th 2016
Courtesy of Prof. Helmut Neumann, University Hospital Erlangen, Germany

In vivo diagnosis of upper GI neoplasia with Optical Imaging (i-scan OE)
Lisbon, May 10th 2016
Courtesy of Dr. Rehan Haidry, University College Hospital London, UK

Brief history of i-scan…and i-scan OE
Lisbon, May 10th 2016
Courtesy of Prof. Dr. Ralf Kiesslich, Wiesbaden, Germany

Imaging Guided Endoscopic Therapy for Early Oesophageal Neoplasia
PENTAX Medical’s UEGW Expert dinner, Camp Nou, Barcelona
Courtesy of Dr. Rehan Haidry, University College Hospital London, UK

Advanced imaging supporting quality in colonoscopy and improving ADR.
32nd GEEW, June 24th 2014
Courtesy of Professor R. Bisschops, UZ Leuven, Belgium

Testimonial 3 - Dr. Alessandro Messi
Courtesy of Dr. Alessandro Messi, Ravenna Hospital, Italy

Testimonial 2 - Dr. Piero Candoli, Ravenna Hospital, Italy
Courtesy of Dr. Piero Candoli, Ravenna Hospital, Italy

Testimonial 5 - Professor Helmut Neumann
Courtesy of Professor Helmut Neumann, UK Erlangen, Germany

Testimonial 4 - Dr. Silvia Sanduleanu
Courtesy of Dr. Silvia Sanduleanu, UMC+, The Netherlands

Testimonial 3 - Dr. Arthur Hoffman
Courtesy of Dr. Arthur Hoffman, HSK Wiesbaden, Germany

Testimonial 1 - Dr Rogier de Ridder
Courtesy of Dr. Rogier de Ridder, Maastricht UMC+, The Netherlands

Normal duodenal architecture
This sequence demonstrates the normal villous architecture of the second part of the duodenum in detail using PENTAX HD+ with i-scan enhancement.
Courtesy of Dr. Rehan Haidry, UCLH, UK

Crohn`s disease duodenum
Crohn’s disease of the upper GI tract is rare and lesions can easily be missed as they are small. i-scan highlights inflammatory changes of the duodenal mucosa and enhances contrast thus making detection of small aphthoid lesions easier.
Courtesy of Dr. Michael Häfner, St. Elisabeth Krakenhaus, Austria

Gastric cancer
This video sequence demonstrates to observe characteristic of surface pattern with i-scan SE then switch to i-scan OE to observe vessel pattern. i-scan OE brought up better assessment of vessel as compared with chromo endoscopy. Following pathological result concluded mucosal cancer 8mm in size.
Courtesy of Prof.Tomoki Michida, Teikyo University, Japan

Gastric cancer
This video sequence demonstrates to observe characteristic of surface pattern with i-scan SE then switch to i-scan OE to observe vessel pattern and demarcation line of lesion without help of magnified scopes. Following pathological result concluded gastric cancer invaded slightly the submucosa.
Courtesy of Prof.Tomoki Michida, Teikyo University, Japan

Radiation Proctopathy (RP)
RP is a chronic condition that has a significant burden on patients quality of life and healthcare. This clip shows how i-scan 2 helps to highlight the vascular lesions in detail in a patient with symptomatic bleeding and allows targeted YAG laser treatment to the lesions. The vascular areas are not prominent on HD WLE or even i-scan 1 but by switching to i-scan 2 thermal therapy can be directed to the abnormal areas.
Courtesy of Dr. Rehan Haidry, UCLH, UK

Ulcerative colitis
In ulcerative colitis i-scan clearly shows inflammatory changes of the mucosa. We also use it in conjunction with chromoendoscopy for the surveillance of patients with longstanding chronic inflammatory bowel disease to increase detection of flat lesions.
Courtesy of Michael Häfner, St. Elisabeth Krakenhaus, Austria

Serrated adenoma
Serrated adenoma are frequently missed as they are flat lesions with very subtle changes to the normal mucosa pattern. i-scan allows for enhanced vision of the vascular pattern and changes like the rim of debris and the mucus cap.
Courtesy of Dr. Michael Häfner, St. Elisabeth Krakenhaus, Austria

Laterally spreading tumour
In this patient with a laterally spreading tumour granular type i-scan was used to get a clear idea about the polyps pit pattern. As a pit pattern type IV was found, indicating a benign lesion, we proceeded to resect the lesion by means of endoscopic mucosal resection.
Courtesy of Dr. Michael Häfner, St. Elisabeth Krakenhaus, Austria

Early gastric cancer
In this video clip i-scan is used to both detect a lesion and to get a clear idea of its margins. Based on i-scan and additional staining with indigo carmine the lesion`s margins were marked and an endoscopic submucosal dissection performed.
Courtesy of Dr. Michael Häfner, St. Elisabeth Krakenhaus, Austria

Hyperplastic gastric polyp
This patient presented with anaemia.
At endoscopy the patient was found to have a large hyperplastic polyp in the stomach. This video sequence demonstrates the characteristic PIT pattern of the hyperplastic lesion using PENTAX HD+ and i-scan enhancement.
This image enhancement was used to direct YAG laser therapy to this area to prevent further blood loss.
Courtesy of Dr. Rehan Haidry, UCLH, UK

Gastric high grade dysplasia
This patient was followed up for a gastric ulcer that had caused a large upper GI bleed. At endoscopy there is a dysplastic antral lesion seen on Pentax enhanced imaging. This lesion was removed by Endoscopic Submucosal Resection.
Courtesy of Dr. Rehan Haidry, UCLH, UK

Crohn`s disease ileum
Aphthoid ulcers of the terminal ileum are a typical finding in Crohn’s disease. As seen in this video, contrast and tone enhancement makes even subtle changes easier to spot.
Courtesy of Dr. Michael Häfner, St. Elisabeth Krakenhaus, Austria

Squamous dysplasia of the oesophagus
Early squamous neoplasia is a very aggressive pathology and the decision when to choose oesophageal sparing local endoscopic resective therapy, over invasive interventions such as surgery, depends on accurate staging. Micro-vasculature in squamous dysplasia is key to informing the endoscopist on the potential depth of invasion. Intrapapillary capillary loops arise from the submucosal veins. This short video clip shows an abnormal area with squamous dysplasia that with the magniview scope and i-scan 2 has type II IPCSLs. The normal vasculature is shown before the abnormal vessels come in to view with zoom imaging. This area was resected by EMR and show M3 invasion alone.
Courtesy of Dr. Rehan Haidry, UCLH, UK

Squamous cell cancer of the oesophagus
Early squamous cell cancer of the oesophagus is easily missed. In these flat lesions, it is also difficult to identify the margins of the tumor. In this patient i-scan was used to assess the extension of the mucosal cancer before performing endoscopic submucosal dissection.
Courtesy of Dr. Michael Häfner St. Elisabeth Krakenhaus, Austria

Early squamous neoplasia of the oesophagus (sq emr)
Early squamous neoplasia of the oesophagus is often very difficult to appreciate with white light endoscopy alone. This patient was referred for assessment of acid reflux symptoms and the referring centre had taken random oesophageal biopsies which reported features consistent with atypia. With enhanced imaging and i-scan, there is an extensive circumferential lesion with abnormal vasculature and mucosal irregularity. With lugol’s chromoendoscopy the extent of the lesion is further appreciated with extensive areas of oesophageal unstaining.
Courtesy of Dr. Rehan Haidry, UCLH, UK

A rare case of malignant melanoma of the oesophagus (Melanoma)
The clip shows a very interesting appearance of the oesophagus. With the various enhancement settings and i-scan, one can see multiple pigmented plaques throughout the tubular oesophagus with areas of hyper-vascularity and dilated tortuous micro-vasculature on i-scan 2. This patient has malignant melanoma of the oesophagus and went on to have an oesophagectomy.
Courtesy of Dr. Rehan Haidry, UCLH, UK

Early oesophageal neoplasia arising in a patient with Barrett`s oesophagus (ACA EMR)
This is a recording of a patient with early Barrett’s cancer. They were referred for radiofrequency ablation. With enhanced imaging and i-scan 1 there is a very subtle nodule with an area of irregularity at the centre.
Courtesy of Dr. Rehan Haidry, UCLH, UK